Tummy Time – A Crucial Neurodevelopment Process
For the purpose of this article we are going to focus our discussion on tongue-ties.
Infant developmental milestones are monitors of how the child’s nervous system is developing and adapting to its environment. During the first two years of life 80—90% of the groundwork for the developing nervous system is being laid down. Synaptic development is advancing at an unprecedented rate (peak development is at 8 months) and is driven by external and internal stimulation. Each milestone is dependent on two things – proper neurological pre-programmed feedback loops and the ability to build on the previous milestone.
We lift our head, we roll over, we sit up, we crawl and creep, we stand and walk. The base of the brainstem, with its pre-programmed proprioceptive feedback loops, is responsible for this process. Along with the motor and sensory development necessary for these milestones to be reached, our social development is also tied into this process. The ability to become more mobile is tied into our ability to explore more of our would, take in more information and begin to codify that input into an adaptive, healthy nervous system. Any interference or interruption to this process will affect the developmental underpinnings of a child’s nervous system, leading to long-term compensatory changes. These changes, especially those established in the first two years of life, can alter a child’s adaptability and neurological thresholds for the rest of their lives.
So, what does this have to do with tummy time and tongue-tie?
Development of balance and coordination is the foundation for postural mechanics that we will depend on for the rest of our lives. This process starts immediately after birth and its foundations are established in the first 18 months of life. Each stage of development must build on the previous stage to allow us to establish an integrated nervous system.
The visual cortex is located in the occipital lobe of the brain (the back and lower portion of the brain). A primitive reflex known as The Visual Proprioceptive Righting Reflex, that is paramount in keeping our brain, eyes and body in relative balance with each other, is triggered as soon as an infant can hold their head up – usually within the first two months of life. By this point in time, an infant consistently relies upon visual clues to orient their head and body. Reflex mediated head control is a primary factor necessary for the progression from holding your head up, sitting, crawling and standing. The sequence of postural development (remember motor and sensory and social development are all intricately bound together) is predicated upon mastering reflex control of the head position relative to gravity.
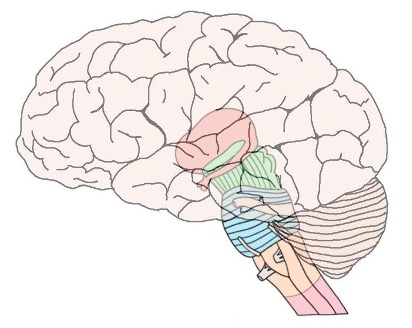
The other portion of the brain that is imperative to normal functional development is the cerebellum. The cerebellum is located just below your cerebrum and behind the upper portion of your brain stem. This is the area at the base of your skull where your head meets your neck. The cerebellum is critically involved in motor coordination and balance. Besides its involvement in motor coordination, it is also implicated in a wide range of other cognitive abilities including: planning, set-shifting, language abilities, abstract reasoning, working memory and visual-spatial orientation. It also has reciprocal projections with the frontal, parietal and occipital association cortex. This, along with the cerebellum’s rapid growth in the first year of life (it grows 240% in the first year) suggests that its proper development is a prerequisite for specific aspects of later cortical development.
Tummy time is an essential developmental activity. There is a direct correlation between brain development and sociological development. When a baby lifts their head up, they are not only developing the secondary curves of their spine (the cervical spine or the neck) they are also developing a different view of the world. Developing those secondary curves is essential to move them from the curled up fetal position to the upright standing position they will use later. Not only that, they develop strength and proper biomechanics as they get more sensory input.
As the baby expands their view of the world, they begin to see and make new connections, thereby increasing their sensory input. All that input goes into their brain, creating movement and sensory stimulus that is essential to the birth of new neurons.
Tummy time is the gateway to proper structural, muscular and neurological development. Posture is largely maintained and propagated by reflexive involuntary control. Much of the reflexive postural control mechanisms are located primarily in the head and neck regions. Visual and vestibular input, as well as receptors in the joints and soft tissue of the spine, play a major role in the regulation of gait and posture. Proper functioning of the aforementioned reflexive pathways sets the stage for the development of the vestibular system. This is a sensory system located in the inner ear that is responsible for providing our brain with information about motion, head position and spatial orientation. It is also involved with motor functions that allow us to keep our balance, stabilize our head and body during movement and maintain posture. This system in congruence with the visual cortex is essential for a host of neurological processes including, balance, muscle tone, alertness, eye movements, processing ability and managing input from the environment to the brain.
At birth we are born with one primary curve in the spine – a U-shaped curve from the neck to the tailbone. As we begin to develop muscle control in the spinal musculature, the secondary curves of the spine form. The first secondary curve to form is the cervical (neck) lordotic (backward) curve. The second one is the lumbar (low back) lordotic curve. The proper formation of these curves is paramount for normal bone growth and modeling as well as dural meningeal tension. The dural meningeal system is made up of three layers of tissue that wrap around the spinal cord, attach to the coccyx, each spinal segment at the dural port – where the nerves exit the spine at the vertebral foramen – at the base of the neck, into the cranium, around the brain and finally to the sutures of the skull. Its function is to maintain proper tension in the central nervous system, facilitate normal cranial and spinal bone growth and allow for the proper movement of cerebrospinal fluid.
If there is traumatization or abnormal development of the suboccipital structures (those structures at the base of the skull and top of the neck) it can inhibit the firing of the pre-programmed proprioceptive feedback loops discussed earlier. If the motor system cannot develop normally, while it is fault tolerant and can overcome considerable impairments, insults or interferences to this system will create compensations in order to adapt to these insults. This will often leave the child with a reduced capacity to take on additional stresses (neurological loads) later in life.
Besides the structural aspects of the developing spine and cranium, there is a soft tissue system known as the fascial system. There is both a longitudinal and transverse set of facial planes. This system is made up of connective tissue that encases our body parts and binds them together. It surrounds muscles, nerves, tendons, and ligaments and gives them shape. Fascia also connects your skin to the tissue that is directly beneath it. For the purpose of this article, the focus will be on the transverse fascial planes. The standard delineation of these transitional planes includes: the occipital-atlantal area, the cervico-thoracic junction, the thoraco-lumbar junction and the lumbo-sacral junction. The transverse diaphragms include the Tentorium Cerebella, The Thoracic Outlet, The Respiratory Diaphragm and The Pelvic Diaphragm. I am going to suggest we include one more: the floor of the palate/mouth. This is the attachment point for the frenulum of the tongue as well as muscle attachments of the mylohyoid, omohyoid, geniohyoid, stylohyoid, genioglossus and digastric. Normal function of these muscles along with the tongue are mandatory for proper swallowing, sucking, jaw movement and head posture.
These muscles along with the frenulum and its relationship to jaw and anterior neck muscle function, play a significant role in an infant’s ability to comfortably experience tummy time. Imagine if your throat and jaw muscles were tight, contracted and unable to stretch comfortably. Now add in the factor that the innervation and musculature at the back of your neck was not fully developed. Think about what it would be like to be laid on your stomach in this situation, unable to comfortably lift your head, not able to use your arms to support you to push up and not able to verbally communicate the challenge or discomfort. This can be the scenario in an infant with aberrant functional tongue, jaw, cervical spine and cranial mechanics.
The ability to nurse, suck, bite, chew and later speak is dependent on a complex system of functional, skeletal, biomechanical and neurological factors. While much of these processes, as stated earlier, are reflexively programmed, improper function and/or structure can have a negative impact on their manifestations. The ability of the jaw to translate forward, backward and laterally as well as to close and open smoothly and correctly is dependent on proper muscle control and balance.
The transverse fascial planes, especially those in the cranium, at the floor of the mouth, the base of the skull and the junction of the neck and upper back if too tense, can transmit this tension and imbalanced forces directly to the underlying muscles and nerves. This tension will set up a compensatory situation as the infant struggles to maintain proper function that is pre programmed into their nervous system. Irritability, unable to suck or nurse correctly, fussiness, colicky symptoms and others can be a result of this imbalance. Since the nervous system and structures that support it, are under stress this situation can also impair proper neurological development including: missed or late milestone timeframes, retained primal reflexes, proprioceptive and processing issues. Lastly, abnormal fascial tension can also affect dural meningeal tension therefore affecting proper bone growth and cerebrospinal movement.
A true tongue-tie (also buccal and lip ties*) that functionally affect the mechanics of the jaw and mouth can also affect palatal bone growth, proper cranial mechanics and development and cervical spine mobility. The hard palate is made up of four bones, two maxillae and two palatine bones. They meet at suture lines that are mobile and can stay that way into the teenage years. If these sutures fuse too soon or incorrectly, they will affect the shape of the palate, mouth, jaw and face. The tongue, dural meningeal system, cerebrospinal fluid motion, fascial attachments and proper muscle control all play a part in the normal functional and aesthetic development of the head, face and neck.
If an infant cannot use their tongue correctly then the translation of the jaw forward, the pressure of the tongue against the palate and the proper bite plane development can be impeded. Not being able to hit all areas of the roof of the mouth equally when nursing or sucking on a bottle, can cause the child to take in air when eating. In addition, unequal pressure on the palate can lead to hypersensitive gag reflexes that can affect eating and feeding. Of course, abnormal tongue movement can play a large part in speech delays or impediments.
There is nothing in a child’s developmental profile that happens in isolation. During those first two years of life the foundations of the nervous system and functional biomechanics are being laid down, at this time the infant’s development is most vulnerable. Tummy time, tongue-tie, craniofacial distortion and spinal biomechanics are all intimately neurologically, biomechanically, physiologically and structurally related. Being aware of the interrelatedness of these parameters, and being able to determine their functional capacity, is paramount for healthcare practitioners and parents to be able to assess the need for interventions that will be best suited for their child’s well-being.
What to do about Tongue-tie?
As you can see from the previous discussion. properly evaluating and treating tongue-tie, along with appropriate follow up care, is extremely important to the health and development of the infant. While revising the tongue-tie itself can often improve function dramatically, regaining lost structural and neurological feedback mechanisms is the purview of integrated care methodologies. Functional rehabilitation of tongue movements serves three purposes: the first is to reduce the possibility of the frenulum reconnecting, secondly, to restore normal muscular control of the tongue, and lastly, to assist in facilitating normal palate development.
Practitioners whose expertise lie in the field of pediatric cranial care can access the functional implications of the tongue-tie, pre-and post-revision, to determine both the necessity and timeframe necessary for corrective interventions. Not all tongue-ties are the same nor do they all have the same implications. Once the tongue-tie is discovered and properly assessed a coordinated effort should be instituted. The longer the tongue-tie was present without corrective intervention, usually the more structural (the cranium and palate) and functional (the tongue and jaw muscles) rehabilitation is necessary.
Cranial adjusting/balancing/correcting is a specific art that requires a skilled practitioner who specializes in this field. In the infant, the sutural system of the cranial vault and base is not formed and the main purpose of the cranial structures, especially in the first two years of life, is to allow for proper brain growth and foundational development of the cranial mechanics. The brain grows 101% in the first year of life and another 15% in the second year. It will grow and average of 21/2– 3 times its size during this time period. At the same time the formation of the palate (while complete fusion may not occur until the early teens) is paramount and dependent on proper cranial bone mechanics, movement of the tongue and jaw, the ability of the child to suck and or nurse correctly and proper swallowing and chewing mechanics. The intricate muscular system of the face, jaw, neck and head, along with fascial and dural meningeal tension membranes, as well as cerebrospinal fluid movement and pressure gradients, are the determining factors is the child’s structural, neurological and functional development.
Cranial adjusting is not about moving the cranial bones but instead it is about being able to address and balance the dural meningeal attachments to the spine and cranium, restoring normal cerebrospinal fluid flow and creating uninhibited neurological pathways to allow underlying preset biomechanical, structural, neurological and functional innate template to express themselves properly. The corrective procedures/adjustments are performed to assist the body in making its own corrections. It is not about moving a bone from point A to point B but instead being able to determine where a corrective force can be instituted to facilitate the body’s attempt to make its own correction.
We as human beings struggle to maintain physical, chemical, neurological and emotional homeostasis. When systems in our bodies are under stress, we make compensations in order to survive and make the best of the situation. Survival needs take precedence. In Infants, food and eating is the basic survival need that usually usurps all others. Therefore, the ability to eat and take in sustenance becomes a primary goal. Anything that interferes with that need will directly affect the infant’s ability to thrive. Nursing and feeding issues, reflux, colic, hypersensitive gag reflexes and later on speech issues, are all signs that proper mechanics of the tongue, jaw and cranium are not working correctly. These structures are intimately related and must be evaluated together. None of these factors are independent of each other.
It is incumbent upon health care practitioners who are working with the repercussions of tongue-tie, in infants, children and adults, to become at the very least, versed in the implications and methodologies involved in working with this patient population. As a specialist and educator in pediatric chiropractic and cranial care for over 38 years I have trained and worked with thousands of chiropractors, chiropractic students, osteopaths and dentists to be able to offer a coordinated, safe and effective approach to the care and treatment of pediatric functional and neurodevelopment issues including tongue-tie and its implications. When working cooperatively with different professions it is important that each practitioner understand and respect the role of their colleague in both the diagnosis and treatment of the problem. The goal as always is to do what is least invasive and most effective to help the patient attain a maximum level of functional improve-ment, both subjectively and objectively.
References
- Sampaio and Truwit, 2001
- Kagan and Herschkowitz, 2005
- Symposium on operative obstetrics, Donn, MD: Vol. 10, No. 2, June 1983
- Major Bertrand DeJarnette, DC “Philosophy Art and Science of Sacro Occipital Technique – 1967
- Retzlaff EW, Michael DK, Roppel RM, Mitchell F, The structure of cranial bone sutures J Am Osteopath Assoc 1976;75:106-7
- Davson H, The blood-brain barrier, The Structure and Function of Nervous Tissue 1972;4.
- Journal of Manual Medicine, Springer – Velag 1992
- Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion. Fernanda Angelieri,a Lucia H. S. Cevidanes,b Lorenzo Franchi,c João R. Gonçalves,d Erika Benavides,e and James A. McNamara, Jrf
- Breig A, Adverse mechanical tension in the central nervous system. New York, NY: John Wiley & Sons; 1978: 11-53.
- Autism, Neurology, Technology A national research network led by UNC School of Medicine’s Joseph Piven, MD, March 2017
- J Am Osteopath Assoc. 2015;115(11):654-665 doi:10.7556/jaoa.2015.136
Featured Articles
View our articles on chiropractic technique, practice management, research and philosophy.